
Diabetes is a chronic disease. For some people, heredity plays a factor. One or more parents or family members may have been diagnosed with either Type I or Type II diabetes. In 2020, the CDC reported there were an estimated 34.2 million Americans currently diagnosed with diabetes. Or roughly 10.2% of people living in the United States.
The Centers for Disease Control and Prevention estimate that only 5.2% of all patients with diabetes have Type I. That is insulin-dependent, where the body is not able to produce its own insulin. While about 1.5 million Americans have Type I, patients with either type of the disease face similar health risks, symptoms, and complications.
Diabetes is considered to be a silent disease. Someone could have the condition for years and not even know it. Some of the symptoms that are an early warning are easily missed. And unless you are testing for diabetes at least once per year, it can be hard to detect. And left unmanaged, diabetes can bring many different health risks. And in the last twenty years, adult cases of diabetes have more than doubled.
If you have been diagnosed with diabetes, managing your blood sugars and making lifestyle changes matter. If you have just found out you have diabetes, the changes you make now could reduce your risk of complications. But knowing, and then actually implementing the right lifestyle changes? That is hard for most people. This is why diabetes is the seventh leading cause of death in the United States.
People living with diabetes have a problem with insulin production. For some, the pancreas cannot produce enough insulin. This is usually the case for people with Type II diabetes. And for others, producing insulin inside the body is no longer possible. And they rely on insulin injections to help their body.
The signs and symptom severity for diabetes increase over time. But in the early days, patients may not know they are developing the condition. Fasting blood glucose is a reliable way to monitor diabetes. And some people who have a family history of the disease measure their blood sugar weekly. It can be an effective early-warning method.
Using a glucometer and a small drop of blood from your finger, you can record and track your blood sugar. If you notice that your average readings are above the expected level for fasting glucose? Talk to your doctor right away about tests to confirm whether you have diabetes.
In the United States, the current guide to healthy blood glucose versus diabetes is:
Source: American Diabetes Association
Some of the early signs to look for are fatigue, dry mouth, and mood variances. People who have high blood sugar can feel anxious. While low blood sugar can feel like exhaustion. Frequent urination is another sign of diabetes.

High blood sugar doesn’t sound like a big problem. But it creates a lot of problems. For example, nerve endings can be ‘burnt out’ over time by high glucose. That is why people with diabetes can develop numbness, particularly in their fingers, hands, toes, and feet. As the nerves are damaged, the ability to sense hot, cold, pressure, and pain are reduced.
Someone with diabetes could have a severe cut on their food getting infected and not even know it. The nerve receptors stop reporting sensations to the brain. Another problem is that high blood sugar causes blockage of the arteries and veins. That also reduces the ability of the immune system to help fight off infections. This can lead to severe skin and wound infection, pressure lesions or sores, and in extreme cases, amputation.
Blood that is high in sugar moves much slower through the circulatory system. And because it is moving slower, it deposits more plaque (or hardened fat and minerals) inside arterial walls. That can reduce the size of veins and arteries, increase blood pressure, and limit the amount of blood circulated through extremities, like hands and feet.
Vision loss is another common risk associated with diabetes. High blood sugar levels can cause damage to the retina of the eye. If it is not diagnosed and treated, people with diabetes can lose their vision. But annual exams with an eye doctor can help with early detection and treatment.
Diabetes is an impairment of the pancreas. The organ that is responsible for making all the insulin your body needs to be healthy. Complete reversal of diabetes doesn’t happen, but when significant lifestyle changes occur, it can slow down and even stop further damage to the body.
When you balance your dietary intake, hydration, and exercise daily, you may find that you need less medication. And some patients can maintain low glucose levels so that they don’t have to take medication at all.
The dietary guide for most people with Type II diabetes is to consume 45 carbohydrates per meal. That is breakfast, lunch, and dinner. And then a 15-carbohydrate snack between breakfast and lunch, and again before dinner.
When people are first diagnosed with diabetes, they learn quickly to avoid high-sugar foods. The big problem is that almost all convenience foods are very high in carbohydrates. Easy meals like pasta? High carb. Breakfast can be one of the most challenging meals of the day. Bread, desserts, jam and jellies, and even fried potatoes are high in sugar.
As you start reading the labels and scrutinizing each food you buy for carbohydrates, sodium (salt), and fiber, the realization happens. That most foods in your local grocery store offer little to no nutritional benefits to your body. And foods like that are quickly converted into more sugar in your bloodstream and stored in fat cells, making it harder to control healthy blood glucose levels.
It’s really about swapping out unhealthy foods that never made you feel full in the first place with better alternatives. And finding carb bargains or foods that are affordable, taste great, and are so high in fiber that the sugar in each serving becomes negligible. Calculate food quality based on net carbs. That is total carbohydrates (per serving) minus the fiber. And always aim for foods that have the lowest carbohydrates possible.
Convenience foods are more expensive. They don’t always taste great, and we know that they can be unhealthy, high in glucose, fat, and sodium. We reach for the foods because we are ‘in a hurry or outside of the house are rarely the best choice for our health. And when you are eating at a restaurant, it is even harder.
People who manage to balance their blood sugar and sustain healthy levels share one secret; they do a lot of meal prep at home. Instead of relying on snacks on the fly, they pack their own when they are outside the house. And they drink lots of water instead of consuming hidden sugars in virtually all popular beverages.
The rushed and hectic schedule of the workweek can make it challenging to prepare food. But if you are at home on a Sunday and relaxing for a couple of hours, you can make it a healthy habit. Plan your lunches and dinners for each day of the week and do some of the meal prep on the weekend to help save time.
Diabetes should never go all day without eating. Low blood sugar can cause some severe health risks. So, it is important for people with diabetes to eat on a regular schedule. Try to front-load foods with higher sugar levels early in the day. That is one secret that can help you burn off sugar and manage your glucose.

Change is hard. Making dietary changes, increasing your exercise and hydration. Smoking cessation is a critical benefit for people living with diabetes. Nicotine and other chemicals in cigarette smoke contribute to arterial hardening and other health complications for people with diabetes.
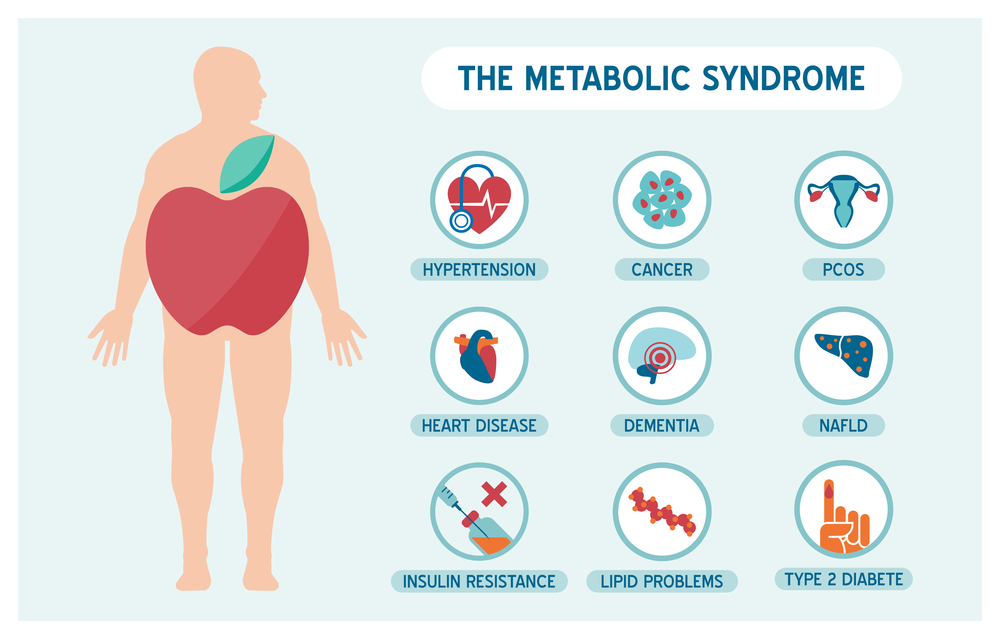
Remember that diabetes is a silent disease. The changes you make today and healthy habits you keep every day reduce your long-term risk for many problems, including:
When it comes to managing diabetes, you have to take the time to manage your health every day. Your primary care provider (PCP) is an asset to you. The physician will monitor your progress and provide suggestions to help you take control of diabetes. With the proper guidance and lifestyle changes, many patients can reduce the risk of developing painful or life-threatening health complications.
Thinking your diet as a person living with diabetes will consist of celery and water? Nope! Thankfully, food science and sweeteners have come a long way. And there are more diabetic-friendly foods available in your supermarket now than ever before.
Does that mean you have to create every meal from scratch? No. The increase of patients with diabetes is slowly changing the American food industry. In the freezer section, you can now find some instant meals that are ‘keto-friendly.’ When you check their label, you’ll notice that keto foods are high in fiber and protein but very low in carbohydrates, making them a perfect meal choice for people with diabetes.
Meal shakes are another excellent standby for people with diabetes. For example, if you work in an office where people bring in donuts to share in the coffee room… bypass. At least most of the time. And if you have a sweet tooth and need a healthier alternative to a dessert, try a nutritional shake instead.
You can keep some in the fridge at work or bring an insulated snack bag to keep them cool. Feeling tempted? Drink down a 2-carb iced coffee protein drink instead. They taste great, and you are getting a full serving of healthy fiber and nutrients.
It is usual for people who are first diagnosed with diabetes to feel anxiety about food. As you start to educate yourself about low-carb food options, however, you can feel like you are entirely restricted. No more good food for you? That’s not the case. But it does take a little more time and effort to prepare healthy and balanced meals.
Don’t get stuck in a food rut! In order to stick to a healthy, low-sugar diet, your food needs to be tasty and delicious too! Otherwise, you are not going to adhere to the low-carbohydrate diet you need to protect your health.
Check out some of our favorite websites for some great low-carb recipes you can try at home.
Natural carbohydrates are healthier than refined ones. That means eating an apple a day or your favorite melon fruit doesn’t have to stop. It may mean choosing a different apple or fruit that is lower on the glycemic (sugar) index. Some types of fruit are higher in fiber and better for people with diabetes. And so are some vegetables.
Every once in a while, you may feel like pigging out. Did you know that four cups of plain buttered popcorn typically count as a 15-carbohydrate snack? Oven-roasted mushrooms with butter and pepper sounds delicious, right? That side dish is considered a ‘freebie’ in carbs, with negligible amounts of sugar. It is about finding new favorite foods that you can enjoy ‘guilt-free while still prioritizing diabetic care.

No one likes to be told what to do. And if your favorite breakfast has been a donut (or two) and a cup of coffee, changing your routine may feel overwhelming. But it’s important to listen to the advice of your PCP (primary care provider) regarding your care.
That means committing to getting your average glucose levels or A1C test every three months. Make sure you take your prescription medications as directed every day. And report any new symptoms to your doctor as soon as possible. Don’t wait until something gets worse before you seek guidance or treatment from your family physician.
If you feel that your family doctor doesn’t offer specialized diabetic care, you can be treated by an endocrinologist. That is someone who specializes in hormone health. The pancreas is the largest gland that is part of the endocrine or hormone system. And problems regulating the insulin hormone can be addressed by a specialist cooperating with your family practitioner.
Some exciting new clinical studies suggest cannabis may help people living with diabetes. Did you know that the human body has built-in cannabinoid receptors? That means cannabinoids (including cannabidiol or CBD) can provide wellness benefits for people diagnosed with diabetes.
One of the most important findings in recent clinical studies is that regular use of cannabis can help improve insulin sensitivity. Cannabis may help make cells in the body more sensitive to insulin. That means each cell can accept insulin and use it more easily. That meant lower fasting glucose levels for some patients who used medical cannabis on a daily basis.
Other studies have suggested that marijuana can help reduce peripheral neuropathy. That means that cannabinoids may help reduce nerve damage that people with diabetes can develop over time. And new studies also suggest cannabis use may help to maintain healthy body weight. Losing weight means that the body needs to use less insulin.
No Information on MarijuanaDoctors.Com should be used to diagnose, treat, prevent or cure any disease or condition. You can view our Full Disclaimer here.