
How much do you know about diabetic neuropathy? You may have a family member or friend with diabetes. Or you may have just been diagnosed with diabetes yourself. About 1 in 10 Americans have been diagnosed with Diabetes. The Centers for Disease Control and Prevention (CDC) estimate that more than 33 million people in the United States have been diagnosed with diabetes.
What is more alarming is the number of people who have prediabetes. That is a condition where blood glucose levels are elevated frequently, indicating insulin resistance. When there is too much glucose (sugar) in the bloodstream, it reduces the ability of cells to use sugar for fuel. Without burning sugar for energy, blood glucose levels continue to get higher. And cause damage to the body.
If the number of Americans with diabetes shocked you, consider that 1 in 3 adults in the United States has prediabetes. According to the CDC, in 2020, that is 88 million more Americans. If patients with prediabetes develop the condition, more than half of the total population in the United States will have diabetes.
Neuropathic pain is one of the most common and debilitating symptoms of diabetes. There are conventional treatments, but they don’t always work. And some of the medications can cause side effects that are almost as bad as the symptoms. Now researchers and physicians are looking at cannabis as an alternative treatment plan for diabetic neuropathy.
When was the last time you had your physician run a blood test for glucose? If you have a great doctor (and good health insurance) after the age of forty-five, that test should be happening on an annual basis. If you have one or more immediate family members with diabetes, annual screening should be done—no matter what age you are.
Statistically, people are at a higher risk of developing type 2 diabetes after forty-five (45) years. That is according to the American Diabetes Association (ADA). And the age that the ADA recommends annual testing.
Diabetes does provide some signs that can help you predict if you will develop a chronic disease in the future. There are several risk factors, including genetics, lifestyle, and other diagnosis, that may provide advanced warning.
Your risk of developing type 2 diabetes is higher if you:
Are from a black, Hispanic, aboriginal, or pacific island heritage
Have a sibling or parent that has been diagnosed with diabetes
Some of the symptoms are simply not noticeable. Diabetes is a chronic disease that, in the initial stages, you have to look for. The symptoms won’t present in a way that makes patients take action.
If something is broken, you will try to fix it. But what happens if something is broken inside your body (or not functioning properly) and you have no idea what is going on? You can’t make the essential changes needed to reduce the harm that diabetes can do to your body if you don’t know you have it.
Early diagnosis of diabetes is critical. If you have been diagnosed with prediabetes, you can make lifestyle changes and take a therapeutic dose of metformin or other insulin medications. That can help improve the performance of your pancreas and delay diabetes and insulin resistance.
When early detection does not happen, high glucose levels start to do considerable damage to the body. The problem is that for years, the damage may not be noticeable. And so, patients don’t always take the diagnosis of diabetes seriously, until they develop symptoms.
You don’t feel diabetic symptoms for the first few years in most cases. Other than frequent urination, dry mouth, and other minor symptoms that are manageable. But once the symptoms do become noticeable and disruptive to your life, the damage is irreversible.
There is no current way to cure diabetes and make it go away. The only tools that patients have are lifestyle changes (low-carb diet, hydration, and exercise) and medications that help stimulate insulin production and make cells less insulin resistant.
Ignoring diabetes is the worst mistake any patient can make. Elevated levels of glucose in the blood cause impairment to nerves, muscles, central nervous system messaging, digestion, as well as reproductive and sexual health. And once the damage is done, there is no way to reverse it. Prevention and early detection are the best weapons patients have to protect their health.
There are many symptoms that someone with type 2 diabetes can experience once they have developed moderate to severe insulin resistance. Diabetic neuropathy is a very misunderstood symptom of chronic disease. It is far more serious than many people realize.
You have probably heard that people with diabetes are at a higher risk of amputations. You may even know someone who lost some toes, a foot, or even a leg to diabetes and sustained a permanent disability. But the exact mechanisms that threaten the health of toes, feet, legs, arms, and hands also threaten major organ functioning.
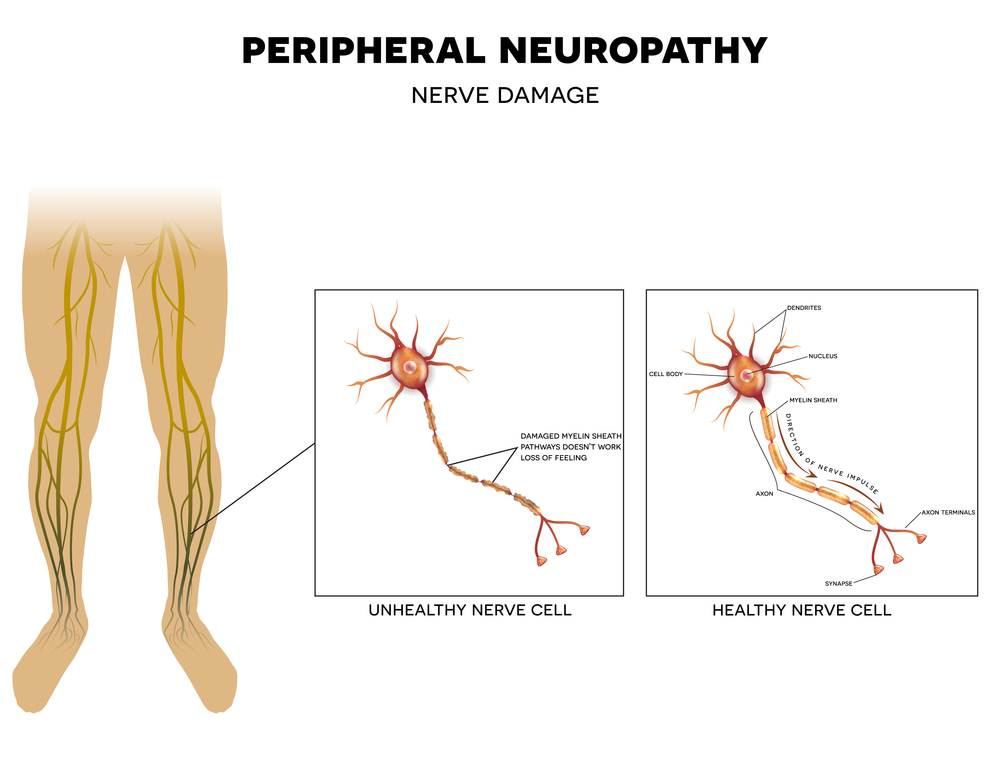
Diabetic neuropathy starts in the extremities for a patient. Most commonly, patients start to experience tingling in their toes. People who have an olive skin tone or darker may experience hyperpigmentation on the toes and feet. This happens because of decreased circulation in the feet, caused by slower blood flow, and more plaque in veins and arteries.
Diabetes thickens the blood. And when that happens, it causes a chain reaction of different health risks. With neuropathy, there isn’t enough oxygenated blood getting to the furthest extremities of the body. That causes a tingling sensation. But it can worsen and feel more like stinging (similar to fire ants) in the toes, hands, and feet—about 50% of people with diabetes experience peripheral neuropathy.
The neuropathy experienced by people who have diabetes can also impact major organs too. It’s not just dealing with numbness in the feet and toes. The same mechanism that restricts blood flow to the feet also reduces blood flow to major organs.
Neuropathy, when you have type 2 diabetes, can cause pain, inflammation, numbness, and impairment to various parts of the body, including:
A significant risk for individuals diagnosed with diabetes is numbness. For example, if you were to sustain a cut on your foot, you would feel it. And then take action to make sure it doesn’t get infected. If the wound did become infected, you would feel that too. Then seek emergency medical care. The numbness from diabetic neuropathy makes wound care and detecting injuries more difficult.
People who have diabetes are also considered to be immune-compromised by the medical community. That is because the impact of neuropathy on every part of the body also impacts immune system functioning. It is easier for people with diabetes to get infections.
Fighting off any infection is hard when you have diabetes. But healing is also compromised. Your immune system counts on strong blood circulation and the production of white blood cells to combat bacteria and viruses. Once someone with diabetes becomes sick, it is harder for them to recover than patients who do not have the condition.

When you have diabetes, the elevation of blood glucose can not only harm your body but can contribute to a variety of mood disorders. Some of the diseases are directly caused by hyperglycemia. While complex emotions can cause others after becoming diagnosed with diabetes.
Getting a diagnosis of diabetes can be very upsetting. Many people don’t understand it. And when you start to learn more about the risk factors, it can be very intimidating. Some people may find lifestyle changes extremely difficult, including weight loss and low-carbohydrate foods. It can also be upsetting to have to start taking medications daily.
Other stressors that patients recently diagnosed with diabetes face are companion chronic diseases and diagnosis. For some women, diabetes could impede fertility, making it difficult or impossible to become pregnant. Loss of vision, neuropathic pain, and other symptoms that can start emerging after the age of forty also disrupt normal life. All the changes can lead to enhanced feelings of anxiety, paranoia, or depression.
High blood glucose levels also do a number on your mood. When blood sugar is low, you may find yourself feeling. Some studies suggest that depression impacts about 25% of all individuals who have diabetes. Glycemic (blood sugar) highs and lows contribute to irritability, or hyperactivity, followed by abnormal fatigue levels.
Fatigue is common when blood sugar levels are not stabilized, contributing to cravings for high-carbohydrate foods for energy—a vicious cycle for someone trying to lose weight.
Doctor-supervised medical marijuana can help moderate many of the symptoms of diabetes. For diabetic neuropathy, cannabis can help reduce inflammation, which may lower the severity of neurological pain. Patients may numb much of the pain; however, cannabis will not help remove sensations of numbness due to nerve damage.
Some studies suggest that the powerful anti-inflammatory benefits of cannabis could also help with insulin sensitivity. Over time, cells become less sensitive to insulin, and that leads to the development of many chronic health risks for diabetics.
In 2016 a study was released that suggested regular marijuana users may have increased insulin sensitivity. It was a large sample study, and physicians revealed that the fasting insulin levels of cannabis users were 16% lower than people who never consumed marijuana. And in the same group, insulin resistance was 17% lower among people who use cannabis regularly.
That’s a big deal.
A recent study also suggested that as the endocannabinoid system (ECS) modulates food intake and energy, people who use cannabis regularly could lose weight. Or maintain a healthy body weight more easily than non-cannabis users.
The study stated: “Modulation of the CB1 receptors with [cannabis] led to a significant reduction in body weight, waist circumference, and triglyceride (TG) concentrations, and an increase in HDL cholesterol, adiponectin concentrations and a reduction in HB-A1C (glucose 90-day average).
Cannabis can help patients with diabetes by making neuropathic pain more manageable. It may also help with symptoms of anxiety or depression, insomnia, and other problems.

When you have a medical card, there are many diverse types of cannabis products you can explore. You may prefer to vape cannabis oil (which is almost odorless and fast-acting). Or you may prefer tinctures (sublingual uptake or drops), edibles, or other intake methods.
If you have neuropathic pain, it can get worse during the evenings. And disrupt your sleep. Both frequent urination and diabetic neuropathy are the leading causes of fatigue or insomnia for patients with diabetes. An Indica tincture can provide both pain and stress relief, helping you sleep through the night without waking up because of pain symptoms.
Topical creams can also be helpful. For many people with diabetes, wounds can take a long time to heal. So, preventing topical infections is a high priority. Cannabis creams and ointments can help with localized pain relief and help keep the skin naturally conditioned to avoid cracks and cuts from dry skin. Cannabis and CBD-infused topicals can be valuable for healthy foot care.
Certain strains of cannabis can provide an elevated mood. These euphoric strains are typically Sativa dominant. They can help moderate feelings of depression and anxiety but also increase energy to combat fatigue that many patients with diabetes experience. Ask your doctor for more information about managing the symptoms of diabetes with medical cannabis.
Right now, no states have listed diabetes specifically as a health condition. However, chronic pain (which is a common symptom of diabetes) is frequently included for patients who want to get a medical card.
Individuals with diabetes are more than twice as likely to develop glaucoma. For states that have legalized medical cannabis, glaucoma is a common symptom included as a qualifying health condition. Patients with diabetes who have developed glaucoma are eligible to apply for a medical card in most states.
Whether you are someone with diabetes who has been diagnosed with clinical anxiety or treatment-resistant depression, you may also qualify for a medical card. And in some states like Louisiana, a physician has the freedom to prescribe medical cannabis for any health condition.
If you have diabetes and are thinking about using cannabis for symptom management, the best place to start is to review your state laws.
Join our patient forum MarijuanaDoctors.com. Our friendly team is available to answer any questions you have about getting a medical card in your state. And provide a referral to a certified physician who can help you apply for your medical card.
No Information on MarijuanaDoctors.Com should be used to diagnose, treat, prevent or cure any disease or condition. You can view our Full Disclaimer here.